
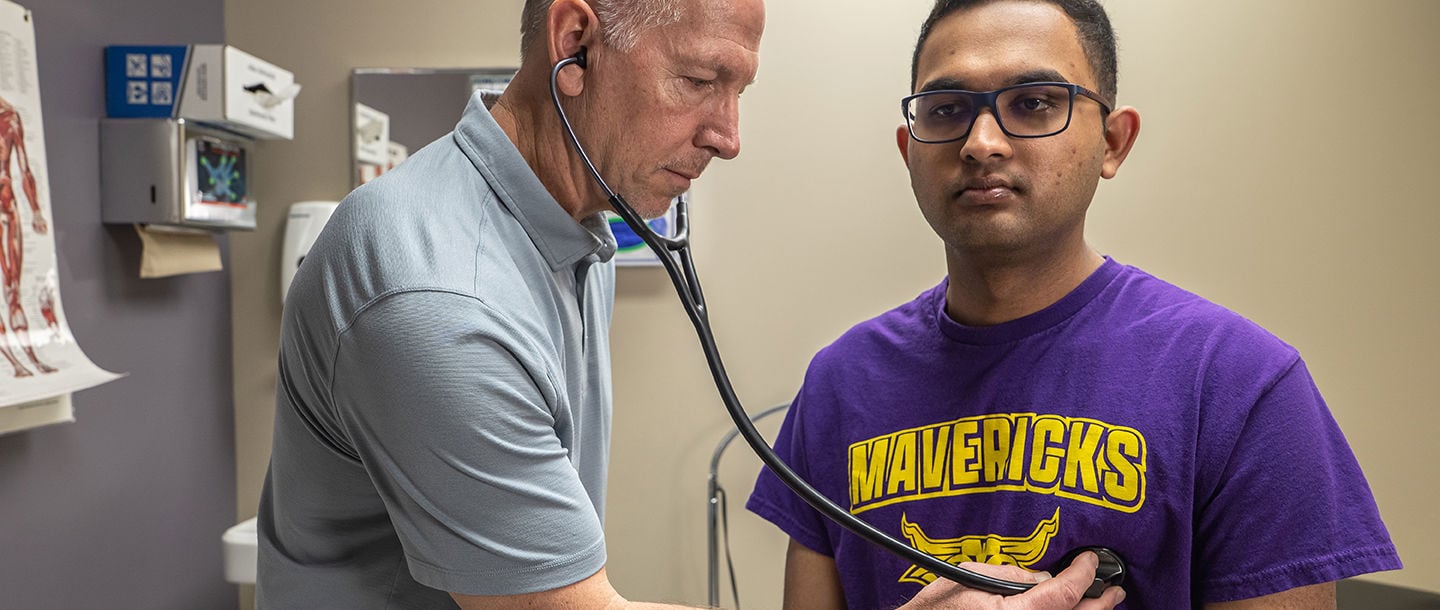





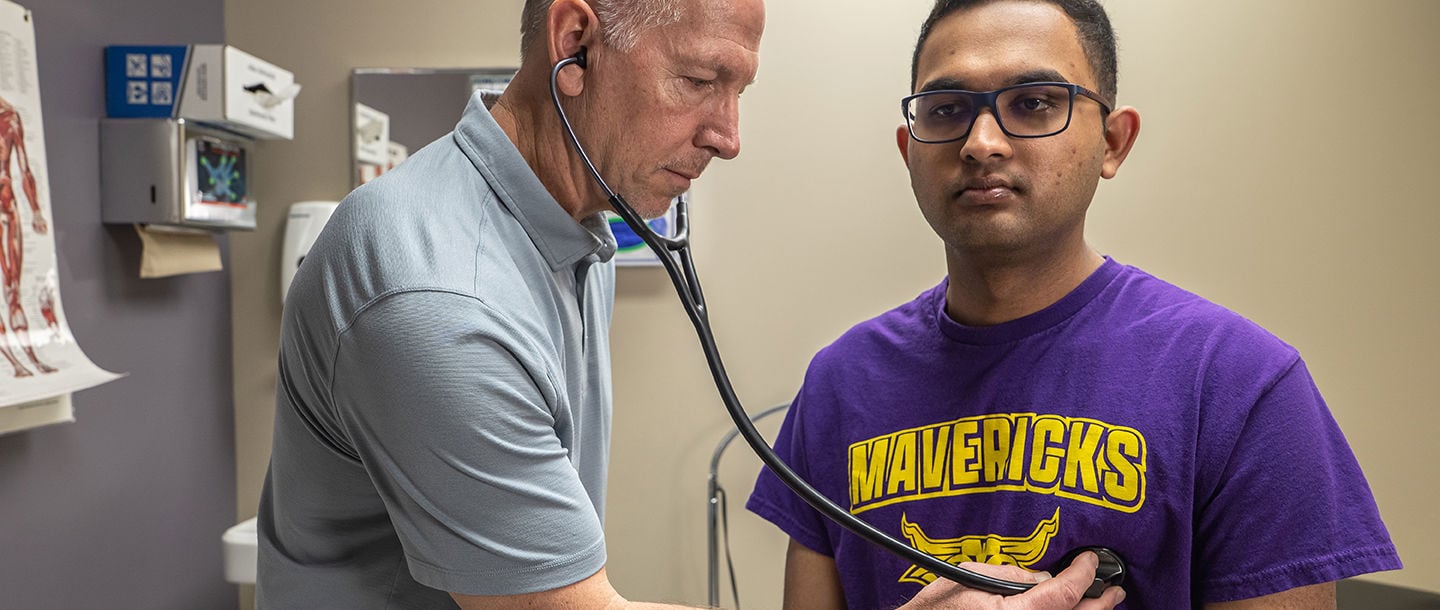



Student Health Services is open for in-person and virtual telehealth appointments. We offer an accredited on-site medical clinic with a full-service pharmacy, lab services and health education. We're here to serve our students! Masks are still required in our facility for patients who have cold, flu or COVID symptoms. If you are sick, please be sure to bring a mask and wear it for your visit.
Student Health Services Medical Clinic provides a variety of health care services to the student population.
Currently enrolled students can take advantage of lower cost prescriptions and over-the-counter medications at our Pharmacy.
The Health Education Office works cooperatively with Student Health Services Medical Clinic to assist students in learning ways to maintain and improve their health.
Instagram and Threads: @msuhealthymaverick
Tiktok: @healthymaverick

21 Carkoski Commons
Minnesota State University, Mankato
Mankato, MN 56001
FAX: 507-389-5787
Student Health Services Medical Clinic and Pharmacy will be open 8 AM to 2 PM, Monday - Friday during the Summer Term (May 13 - July 19). Students may schedule an appointment by calling 507-389-6276 or by visiting the Patient Portal.
Minnesota State Mankato Student Health Services Medical Clinic provides quality and affordable medical services for students.
The Student Health Services Pharmacy dispenses prescriptions and over-the-counter (OTC) medications and supplies at a lower cost to currently enrolled students. We are here to support students by keeping them healthy.
The Health Education Office offers a variety of services, and staff and volunteers are available to assist students with campus-wide health promotion, alcohol and drug education, peer education activities, and more.
The Student Health Services Lab can perform both simple and complex laboratory tests including tests for Strep, pregnancy tests, urinalysis tests, blood tests, and STD screenings.
Forms needed for Student Health Services clinic visits and services can be found on this page.
Minnesota State Mankato Student Health Services provides quality and affordable medical services and health education to our University students to enhance their learning experience and support their academic success.
This Contact Us form is for general inquiries or administrative questions only. Call 507-389-6276 during clinic hours for an appointment or personal medical questions. For emergencies, contact Campus Security at 507-389-2111 or dial '911'.